Source: https://hillnotes.ca/2020/10/30/long-term-care-homes-in-canada-the-impact-of-covid-19/
Revised on 5 January 2021, 11:50 a.m.
Any substantive changes in this HillNote that have been made since the preceding issue are indicated in bold print.
(Disponible en français : Les répercussions de la COVID-19 sur les foyers de soins de longue durée au Canada)
According to the National Institute on Aging (NIA) at Ryerson University, by 5 January 2021, long-term care (LTC) and retirement homes reported 11% of the Canadian totals of COVID-19 cases and 73% of total deaths.
This HillNote describes the impact that COVID-19 has had on Canada’s long-term care home residents and staff, and subsequent recommendations and initiatives.
For more information, please see: Long-Term Care Homes in Canada – How are They Funded and Regulated?
COVID-19 in Canada’s Long-Term Care Facilities
The largest proportion of COVID-19 cases in Canada has been in individuals aged 20-29 years. The smallest proportion has been among people aged 70-79 years. However, most deaths from the disease have been among older Canadians – 71% among people 80 years and older, and almost 97% among individuals 60 years and older.
Proportion of COVID-19 Cases and Deaths by Age in Canada
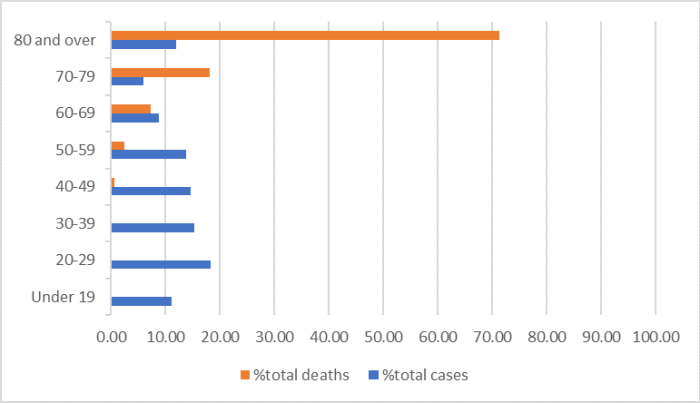
Source: Prepared by author based on data from Government of Canada, Situational Awareness COVID-19 Dashboard, accessed 14 October 2020.
While individuals 80 years and older represent 12% of all COVID-19 cases, they make up 71% of the deaths.
Proportion of COVID-19 Cases That Have Been Fatal, by Age Range
Source: Prepared by author based on data from Government of Canada, Situational Awareness COVID-19 Dashboard, accessed 14 October 2020.
In June 2020, the Canadian Institute for Health Information reported that Canada had a higher proportion of COVID-19 deaths within LTC settings than other OECD countries included in its comparison. At that time, deaths in Canadian LTCs from COVID-19 were at 81% of the total, while OECD countries reported LTC COVID-19 deaths of 10-66% (average of 38%) of their totals.
The report noted that “comparisons must be interpreted with caution due to rapidly evolving infection case numbers, different definitions of LTC and variations across countries in COVID-19 testing and reporting practices.” As well, it found that a larger proportion of Canada’s seniors live in LTC homes and that the LTC population is older than the residents of LTC facilities in comparator countries. Finally, it stated that Canada’s LTC facilities had fewer health care workers per 100 residents than the OECD average.
As noted above, the NIA indicated that to date, 11% of COVID-19 cases and 73% of all COVID-19 deaths in Canada have been in LTC facilities, affecting both residents and staff. NIA’s summary also revealed that 82% of all COVID-19 cases within LTC facilities in Canada, and 88% of deaths, were in Ontario and Quebec.
Summary of COVID-19 Cases and Deaths in Long-Term Care Facilities in Canada
| Total COVID-19 Cases in Canada | 513,543 |
| Total COVID-19 Deaths in Canada | 14,291 |
| Total Long-Term Care Homes | 5,801 |
| Number of Long-Term Care Homes with COVID-19 Cases | 2,171 |
| Number of COVID-19 Cases among Residents | 37,513 |
| Number of COVID-19 Cases among Staff | 17,424 |
| Percentage of all COVID-19 Cases that are in Long-Term Care facilities | 11% |
| Number of Long-Term Care Resident Deaths from COVID-19 | 10,450 |
| Number of Long-Term Care Staff Deaths from COVID-19 | 16 |
| Percentage of all COVID-19 Deaths that have been in Long-Term Care facilities | 73% |
Source: Prepared by author based on the National Institute on Aging, Long-Term Care COVID-19 Tracker, Canadian Summary, accessed 5 January 2021.
2016 census data indicates that 121,140 individuals over the age of 80 years lived in nursing homes, of whom 73% were women. While there is no national data that provides a gender breakdown of COVID-19 cases or deaths in LTC facilities, Ontario reported that 64.5% of COVID-19 cases among LTC residents were women. The data reveals that men are more likely than women to die of COVID-19 in LTC homes, as is the case in the general population.
The Impact of COVID-19 on Long-Term Care Operations and Staff
The high proportion of COVID-19 deaths among elderly individuals living in LTC homes has exposed long-standing challenges in the delivery of long-term care in Canada. In April 2020, the governments of Quebec and Ontario each requested assistance from the federal government to manage COVID-19 outbreaks at LTC facilities.
In response, the Canadian Armed Forces (CAF) deployed teams to 20 facilities in Quebec and five facilities in Ontario. The CAF submitted reports to both provincial governments. Both the Ontario and Quebec [in French] reports noted insufficient supplies of personal protective equipment, poor quality of care, chronic understaffing and inappropriate behaviour towards residents. It has been noted that many facilities could not allow for sufficient physical distancing and could not implement isolation protocols. Ontario and Quebec [in French] ordered investigations into the impact of COVID-19 on LTC homes. Ontario’s Long-Term Care COVID-19 Commission issued interim recommendations on 23 October 2020, which included recommendations to increase the levels and mix of staffing in LTC homes, improve infection prevention and control measures, and allow family and caregivers to visit LTC residents.
A June 2020 report on LTC home staffing by the Royal Society of Canada stated that “[t]he pandemic just exposed long-standing, wide-spread and pervasive deficiencies in the sector” and made nine recommendations to address “the workforce crisis in nursing homes”, urging “coordinated leadership” between the federal and provincial/territorial governments.
The report noted that nurses are the primary regulated health care professionals within LTC facilities, with physicians rarely on site. It found that nurses provide little direct care to residents and that up to 90% of direct resident care is provided by unregulated and unlicensed care aides or personal support workers. The report noted that care aides often:
- receive low wages;
- receive minimal and variable education across the country;
- work part-time without benefits;
- are contracted through agencies and are unfamiliar with the LTC facility where they work; and
- are not included in decision-making and family conferences, despite spending the most time with residents.
Further, the report revealed that care aides have high levels of work-related stress and are at risk of burn-out. The following statistics describe LTC care aides:
- almost 90% are women, 70% of whom are older than 40 years, often from racialized and marginalized groups;
- 60% speak English as a second language;
- some 50% working in urban centres are immigrants;
- 25-30% work more than one job; and
- 65% report having insufficient time to properly complete care tasks.
The report included recommendations for national standards for staffing and infection control training and resources. It further called for increased federal funding to support the provinces and territories to implement national standards, and recommended changes by provincial and territorial governments including:
- appropriate, equitable and permanent pay and benefits, including sick leave for care aides;
- mental health supports for all staff; and
- improved and required data collection.
A number of stakeholders are urging the federal government either to specifically include LTC in the Canada Health Act or to implement separate legislation on LTC that would include national standards.
Recent Federal Activities
The federal government issued guidance for LTC homes for infection prevention and control of the coronavirus. A federal Task Force on Long-Term Care was created by Canada’s Chief Science Advisor, and a report was made public on 30 October 2020.
The Safe Restart Agreement announced in September 2020 includes $740 million dollars for LTC, home care and palliative care to support one-time costs during the pandemic. As well, the federal government’s Speech from the Throne that same month included a commitment to work with provinces and territories to establish national standards for LTC and to “take additional action to help people stay in their homes longer.”
Author: Sonya Norris, Library of Parliament